As part of a month of events in the lead up to International Women’s day, Health Systems Global’s thematic working group on community health workers (CHWs), CHW Central, REACHOUT, and RinGs, held a webinar: “CHWs: the gender agenda”. There is a blog on the presentations and discussions. The purpose of this post is to answer some of the insightful questions our participants posed.
Chaired by Asha George, JHSPH, the webinar started with an overview from Sally Theobald, LSTM, of the issues and context surrounding gender and CHWs, highlighting their importance in addressing sustainable development. This was followed by case studies from conflict-affected settings, Amuda Baba Dieu-Merci, IPASC and Hana Rabadi, World Vision gave examples from DRC and Palestine respectively. There was a huge level of engagement from our participants from around the globe, who commented on parallels in the roles, challenges and contextual issues demonstrated by our case studies within their own diverse country contexts, from Uganda, Kenya, Nepal, India, Afghanistan to the US.
So, let’s start at the beginning:
What is the composition of CHWs by gender globally?
There is a need for greater reporting here as the evidence base is very dependent on the definitions we use; while an older literature review found that among those studies that disaggregated data, programs were reported to be female dominated, subsequent studies focused on CHWs for sick children found that national programs in sub-Saharan Africa had mixed gender compositions.
What are the benefits/limitations of having male or female CHWs in terms of the specific health activities they can carry out?
A review of the literature shows the need for further context based evidence on how gender influences. In Uganda, CHWs in a RinGs and FHS photovoice project documented that male CHWs perform better, in certain roles such as responding to emergencies, mobilising the community for public health interventions and engaging in manual activities such as clearing drainage of water sources.
However, one of the key issues with having a male or female CHW is client preference for receiving services. One participant offered an example from a CHW programme in Zambia, which demonstrated that clients expressed a preference for receiving services, particularly for sexual and reproductive health services, from a provider of the same sex, and this is echoed throughout the literature. Research from Tanzania showed that male and female CHWs performed equally well in maternal, newborn and child health promotion, but women who were married and had had children of their own were more accepted by other mothers. In this way, it is pertinent to consider the gender in recruitment of CHWs – if the focus is on maternal health it probably is justified to have an all female by policy cadre of CHWs, but in doing this, are we neglecting the role of men in pregnancy and associated care seeking and more broadly the health of the men in the community? The same study in Tanzania found that male CHWs were more acceptable for addressing male health issues, particularly those related to sexual and reproductive health, a study in Brazil found that addressing STIs and domestic violence among pregnant women, could not be done without male engagement.
The next question is one we’re glad came up – are there any tools or policy guidelines to help countries make strategic decisions about CHW gender based on their expected roles and responsibilities and on the context?
The simple answer, to the best of our knowledge, is no. Whilst policies may acknowledge gender responsiveness to an extent in their guidelines, there are no hard or fast recommendations, simply because this is an emerging topic and not enough research has been done is this area yet.
However, it is important gender is considered in policy as the development of policies and guidelines addressing the gendered experience of the CHWs may also aid us in answering some of the other questions that arose regarding scale-up of using CHWs to address gender–related barriers in access to care and the successful integration of CHWs into the formal health sector.
CHW attrition rate and discontinuity in service provision has been a key concern within the industry; how do we ensure programme sustainability and continuity of service provision among CHWs?
Attrition and discontinuity has long been an issue, and whilst it is ultimately an individual’s decision to stop work as a CHW, some of the literature suggests that competing demands on a woman’s time, lack of spousal support and lack of proper remuneration have a role to play. Policies that promote payment of CHWs may also have unintended gendered consequences. In Mozambique, while the revitalized CHW policy had an explicit preference for women, communities selected men because they felt men were more deserving of ‘paid’ work. Similar dynamics were also found in Burkina Faso. Attrition rates among male CHWs in Mozambique are also high, as men tend to drop-out in favour of higher salaried positions to fulfill their ‘breadwinning’ role.
Additionally, supportive supervision is vital in solving this issue, however, when men occupy most supervisory positions, female CHWs often don’t see that they have room for progression, or an obvious career path and may become demotivated. Again, the need for guidelines and policies acknowledging these gender-related challenges would be incredibly beneficial.
Questions about the DRC
What sort of relationship do CHWs have with health facility health workers? Has their increased influence in the communities had any negative impact on their relationship with health workers?
In the DRC normally CHWs have a very good relationship with health facility health workers as the chief nurse is invested in the selection process of CHWs with staff from health district. They have regular meetings with health centre staff to see how they can improve their work. Their increased influence in the communities has very positive impact on their relationship with health facility workers as nurses consider that the population health indicators improve through the work of CHWs. CHWs and health facility workers meet regularly in health centre to discuss, plan, monitor and evaluate.
In DRC, to what extent do community health programmes engage other community stakeholders? Has this influenced community and government buy-in and commitment, and therefore sustainability?
For each different community health programme involving CHWs, different community stakeholders are associated from the planning phase. Delegates from community health committee, traditional institutions and social groups such as women’s groups from different health-centre catchment areas, discuss health problems and try to identify solutions. Then CHWs make a plan to address the problem. This level of ownership means there is a high commitment of different stakeholders, which facilitates the sustainability of the interventions.However, specific programmes, such as Expanded Programme of Immunisation may have greater sustainability issues than others.
Many community health programmes targeting mothers and newborn are donor-funded (and sometimes donor-driven). This raises the issue of sustainability when donors pull out. What are the lessons learnt from the Congo?
Yes, many community health programmes targeting mothers and new born are donor funded and there can be the issue of sustainability when they pull out. However, in DRC, CHWs are not programme-focused, they have a holistic role in the community and are involved in different community-based activities. Furthermore, the CHWs come from the communities they serve so they are willing and committed to helping their communities. Aside from CHWs there are also other measures in place, such as mothers’ groups, which have been highly successful in sustaining the programme.
Questions about Palestine
Relating to CHWs in Palestine’s health system participants were interested to know how CHWs address security challenges during home visits?
The presentation was mainly focussed on CHWs from West Bank, which is considered a less fragile context comparing to Gaza but measures to ensure security are that CHWs have been selected from the same communities they serve so they can easily and safely deliver their services. The CHWs programme in Gaza was only introduced few months ago so there are no clear details as yet however, due to the specific context, the CHWs have been trained on how to shift from normal interventions to crisis interventions and they have also been trained in first aid.
Given that CHWs are predominately women, who are particularly vulnerable in fragile and conflict affected states this is clearly an important area for lesson sharing across contexts.
Regarding the transformative role and empowerment of CHWs as demonstrated in West Bank, participants were interested to find out, whether the empowerment was an intended side effect and what the indicators for measuring change were in the CHWs themselves?
The main aim of this program was to improve and maternal child health outcomes so we didn’t have clear indicators for empowerment at the beginning. The personal changes were beyond our expectations but during the implementation we noticed huge changes regarding community norms, gender and empowerment and we started discussing these changes with the CHWs to learn more about the impact of this program from a different angle. Data was collected from the CHWs and their families through personal interviews only, in addition to our observations.
In Palestine CHWs are now officially registered with the directorates of health supporting government’s health teams in activities such as growth monitoring, vaccination and awareness raising. The transformation CHWs in West Bank experienced is not unique to Palestine with a participant from Uganda commenting that CHWs in East Central Uganda have recognised their role as a potential conduit into local politics. These unintended consequences of CHW programmes are fascinating and would benefit from further exploration.
Participants also recognised the importance of buy-in from other community stakeholders to address health and gender issues and asked: to what extent are other community stakeholders involved in the day-to day activities?
Hana Rabadi commented that in Palestine they have the following groups involved:
-
Community active groups (CAGs) who support the CHWs when needed
-
Disaster risk reduction groups (DRR) whose main role is to support and provide services during emergency situations they usually coordinate and work closely with the civil defense
-
Male and Female faith leaders support in delivering messages and organizing related activities
So there you have it.We hope that helps answer some of your questions, and inspires you to think about these gendered issues in your own research. In the meantime we look forward to welcoming you back for the next event in the lead up to International Women’s day 8th March. Watch this space.
Further reading and resources:
Chilundo, B. G., Cliff, J. L., Mariano, A. R., Rodriguez, D. C. and George, A. (2015) ‘Relaunch of the official community health worker programme in Mozambique: is there a sustainable basis for iCCM policy?’, Health Policy Plan, 30 Suppl 2, pp. ii54-ii64.
Daniels K, Odendaal WA, Nkonki L, Hongoro C, Colvin CJ, Lewin S. Incentives for lay health workers to improve recruitment, retention in service and performance (protocol). Cochrane DB Syst Rev. 2014;7.
Feldhaus, I., Silverman, M., LeFevre, A. E., Mpembeni, R., Mosha, I., Chitama, D., Mohan, D., Chebet, J. J., Urassa, D., Kilewo, C., Plotkin, M., Besana, G., Semu, H., Baqui, A. H., Winch, P. J., Killewo, J. and George, A. S. (2015) ‘Equally able, but unequally accepted: Gender differentials and experiences of community health volunteers promoting maternal, newborn, and child health in Morogoro Region, Tanzania’, Int J Equity Health, 14, pp. 70.
George, A. (2008) ‘Nurses, community health workers, and home carers: gendered human resources compensating for skewed health systems’, Global Public Health, 3(sup1), pp. 75-89.
George, A., Theobald, S., Morgan, R., Hawkins, K. and Molyneux, S. (2015) ‘Snap shots from a photo competition: what does it reveal about close-to-community providers, gender and power in health systems?’, Human Resources for Health, 13, pp. 57.
George, A., Young, M., Nefdt, R., Basu, R., Sylla, M., Clarysse, G., Bannicq, M. Y., de Sousa, A., Binkin, N. and Diaz, T. (2012) ‘Community health workers providing government community case management for child survival in sub-Saharan Africa: who are they and what are they expected to do?’, Am J Trop Med Hyg, 87(5 Suppl), pp. 85-91.
Give, C. S., Sidat, M., Ormel, H., Ndima, S., McCollum, R. and Taegtmeyer, M. (2015) ‘Exploring competing experiences and expectations of the revitalized community health worker programme in Mozambique: an equity analysis’, Human Resources for Health, 13(1), pp. 1-9.
Kok, M. C., Kea, Z. A., Datiko, D. G., Broerse, J. E. W., Dieleman, M., Taegtmeyer, M. and Tulloch, O. (2015) ‘A qualitative assessment of health extension workers’ relationships with the community and health sector in Ethiopia: opportunities for enhancing maternal health performance’, Human Resources for Health, 13(1), pp. 1-12.
LeFevre, A. E., Mpembeni, R., Chitama, D., George, A. S., Mohan, D., Urassa, D. P., Gupta, S., Feldhaus, I., Pereira, A., Kilewo, C., Chebet, J. J., Cooper, C. M., Besana, G., Lutale, H., Bishanga, D., Mtete, E., Semu, H., Baqui, A. H., Killewo, J. and Winch, P. J. (2015) ‘Profile, knowledge, and work patterns of a cadre of maternal, newborn, and child health CHWs focusing on preventive and promotive services in Morogoro Region, Tanzania’, Human Resources for Health, 13(1), pp. 1-14.
Lehmann U, Friedman I, Sanders D. Review of the Utilisation and Effectiveness of Community-Based Health Workers in Africa. University of the Western Cape, South Africa; SEED Trust, South Africa. 2004. http://www.rmchsa.org/wp-content/resources/resources_by_theme/MNCWH%26NSystemsStrengthening/ReveiwUse%26EffectivenessOfCHWsInAfrica.pdf [Accessed on 2 December 2015].
Lunsford, S. S., Fatta, K., Stover, K. E. and Shrestha, R. (2015) ‘Supporting close-to-community providers through a community health system approach: case examples from Ethiopia and Tanzania’, Human Resources for Health, 13(1), pp. 1-9.
Mahmud, I., Chowdhury, S., Siddiqi, B. A., Theobald, S., Ormel, H., Biswas, S., Jahangir, Y. T., Sarker, M. and Rashid, S. F. (2015) ‘Exploring the context in which different close-to-community sexual and reproductive health service providers operate in Bangladesh: a qualitative study’, Human Resources for Health, 13(1), pp. 1-10.
Mpembeni, R. N. M., Bhatnagar, A., LeFevre, A., Chitama, D., Urassa, D. P., Kilewo, C., Mdee, R. M., Semu, H., Winch, P. J., Killewo, J., Baqui, A. H. and George, A. (2015) ‘Motivation and satisfaction among community health workers in Morogoro Region, Tanzania: nuanced needs and varied ambitions’, Human Resources for Health, 13, pp. 44.
Naimoli JF, Perry HB, Townsend JW, Frymus DE, McCaffery JA. Strategic partnering to improve community health worker programming and performance: features of a community-health system integrated approach. Human resources for health. 2015;13:46.
Ndima, S. D., Sidat, M., Give, C., Ormel, H., Kok, M. C. and Taegtmeyer, M. (2015) ‘Supervision of community health workers in Mozambique: a qualitative study of factors influencing motivation and programme implementation’, Human Resources for Health, 13(1), pp. 1-10.
Raven, J., Akweongo, P., Baba, A., Baine, S. O., Sall, M. G., Buzuzi, S. and Martineau, T. (2015) ‘Using a human resource management approach to support community health workers: experiences from five African countries’, Human Resources for Health, 13(1), pp. 1-13.
Sacks, E., Alva, S., Magalona, S. and Vesel, L. (2015) ‘Examining domains of community health nurse satisfaction and motivation: results from a mixed-methods baseline evaluation in rural Ghana’, Human Resources for Health, 13(1), pp. 1-13.
Saprii, L., Richards, E., Kokho, P. and Theobald, S. (2015) ‘Community health workers in rural India: analysing the opportunities and challenges Accredited Social Health Activists (ASHAs) face in realising their multiple roles’, Human Resources for Health, 13(1), pp. 1-13.
Turinawe, E. B., Rwemisisi, J. T., Musinguzi, L. K., de Groot, M., Muhangi, D., de Vries, D. H., Mafigiri, D. K. and Pool, R. (2015) ‘Selection and performance of village health teams (VHTs) in Uganda: lessons from the natural helper model of health promotion’, Hum Resour Health, 13, pp. 73.
Vaughan, K., Kok, M. C., Witter, S. and Dieleman, M. (2015) ‘Costs and cost-effectiveness of community health workers: evidence from a literature review’, Human Resources for Health, 13, pp. 71.
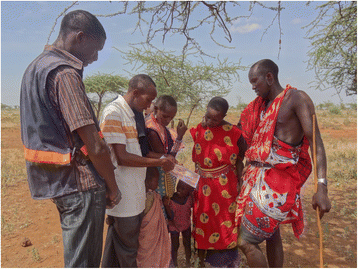
Photo credit: Overseas Strategic Consulting, Ltd.
Read the article